Mood, mental health, and the microbiome
I believe that most, if not all people, have felt the heavy and restricting emotional stagnation brought on by depression, anxiety and brain fog at some point. Presents differently for everyone, but the unhealthy results erode away at our quality of life.
Imagine the racing thoughts, like an endless, unchangeable screen, keeping you awake every night for hours. Waking up in a blink, feeling like you never even slept. Brain fog is so bad you walk into the kitchen, not even remembering why you were there. Physical symptoms like abdominal bloating, diarrhea and body aches. You blame it on getting older even though in the back of your mind you know something is wrong. Mood and mental health disorders are complex and varied, and effective treatment goes beyond just suppressing symptoms with medication.
My interest in the gut or GI tract began during my early years of medical training, when I treated many patients with irritable bowel syndrome. Patients would come in with alternating constipation and diarrhea, abdominal bloating, abdominal pain and cramping. They would ask for a medication to help manage their symptoms. In time, I noticed a trend. These patients would also suffer from mental health or mood disorders. Like depression, anxiety, or chronic stress. Their digestive problems were a sign of a deeper issue, and their symptoms got worse when they were under mental stress, even while taking medication.
Still to this day, we don't fully understand the exact mechanism of IBS, but the current theory suggests multiple factors contribute to the disruption of the gut-brain axis. We do, after all, have a second brain in our gut, so to speak.
Why the focus on IBS? Well, 50-90% of IBS patients suffer from mental health problems and 40-60% fall under the diagnosis of mood or psychological disorders.
The discovery of the GUT-brain axis in germ-free mice has revealed its crucial role in coordinating endocrine, neural, and immune functions, highlighting a complex interplay between these systems.
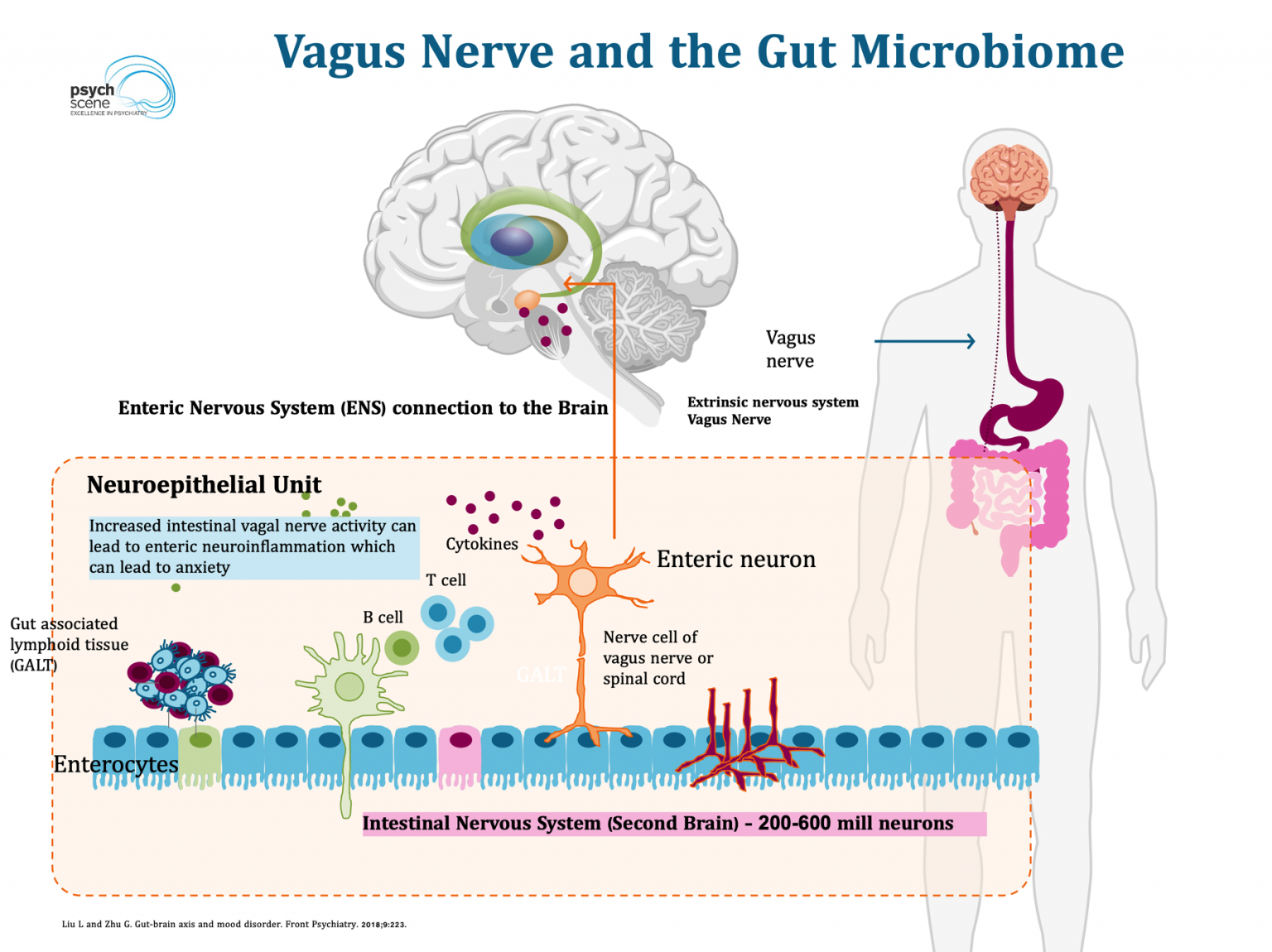
It would make sense the second brain connects deeply with regulation of our emotional system and the brain. Anything that breaks or weakens communication with this system wrecks havoc on our emotional and mental wellbeing.
It is crucial to treat the underlying cause and not treat the symptoms. IBS is the body telling the brain hey we need to fix our second brain.
Many factors play a role in the disruption of the gut brain axis. We mainly focus today on nutrition and the microbiome.
Research shows there are bad bacteria (Bacteroidetes, Proteobacteria, and Actinobacteria) found in higher proportions in patients with major depressive disorder and less good bacteria (Lactobacillus, Bifidobacterium) probably contributing to many of the gut and mood/mental health symptoms.
While the diversity of our microbiome population diversity grows and flourishes because of multiple factors from birth and early childhood, we can still alter the bacterial population with changes in diet. For example, children with seizure disorders who follow a ketogenic diet experience significant changes in their microbiome, often resulting in a reduced frequency of seizures. In the emerging field of nutritional psychology, nutrition provides a bridge to a cure, rather than a bandaid to manage symptoms.
Three simple changes
Fermented foods
Contain rich probiotics and live bacteria which are healthy for the microbiome. The microbiome feeds on fermented foods forming far more diverse populations which reduce inflammation linked to anxiety and depression. The beneficial bacteria interact with the vagus nerve and produce neurotransmitters essential for mood regulation preventing anxiety and depression. Probiotic-rich diets have been associated with reduced symptoms of depression and anxiety in clinical trials.
Healthy fats
Omega-3 fats are crucial for healthy guts, brains, and inflammation prevention. Healthy fats, like omega-3s, can reduce neuroinflammation, a major contributor to depression and anxiety. Studies link omega-3 supplementation to improvements in depression, particularly when paired with probiotics. Omega-3 fatty acids affect mood and behavior, and low blood levels are associated with depression and pessimism.
Up your Protein intake
When we eat protein, the bacteria in the gut creates break down products called short chain fatty acids (SCFAs). The anti-inflammatory properties of SCFAs, like butyrate, strengthen the gut barrier and prevent inflammation. Researchers have linked adequate protein intake to reduced gut inflammation and enhanced neurotransmitter synthesis, which can ease symptoms of anxiety and depression. One study found higher fat and protein intake correlated with lower anxiety and depression whereas with higher consumption of carbohydrates lead to increased levels of stress, anxiety and depression.
Avoid processed food
The list of harmful toxins and artificial compounds in processed foods is endless. Emulsifiers, artificial sweeteners, and refined sugars lays waste to the diversity of the microbiome and promote an environment of unhealthy gut bacteria. Systemic inflammation and gut issues ensue. A study in Nature (2015) demonstrated that emulsifiers commonly found in processed foods promote gut dysbiosis and low-grade inflammation, both of which impair the gut-brain axis. Diets low in processed foods improve microbiome diversity and gut integrity, correlating with better mental health outcomes.
Putting it all together
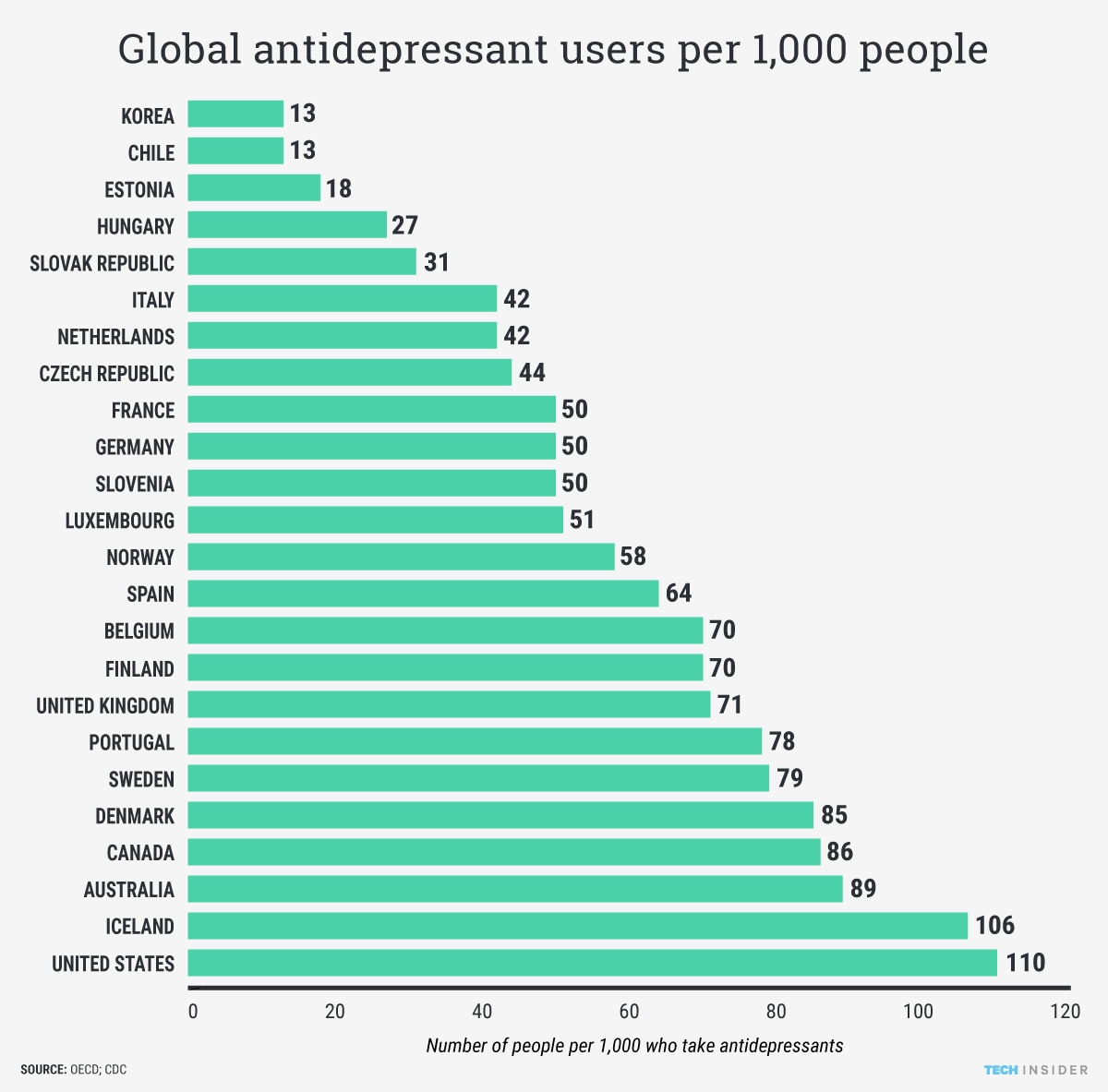
The second brain working with a colony of over 3 billion bacteria seems like the plot from an up and coming second rate sci-fi movie, but it can make all the difference between feeling down in the dumps vs flying high above the clouds. Antidepressant usage in the United States is significant and has been steadily rising. Approximately 13.2% of adults aged 18 and over reported taking antidepressant medications, as of 2015–2018 data. This accounts for nearly 1 in 8 adults, with women, particularly those over 60, showing even higher rates, about 24.3% in this age group. Let's be honest. While fixing mental and emotional well-being may not be as straightforward as simply altering gut health, it could significantly improve your overall health and well-being.